By Jana Manolakos
At this very moment, squiggling and squirming inside your gut are millions upon millions of tiny strands of bacteria that scientists believe may hold the key to understanding inflammatory bowel disease (IBD) and human health.
As a trailblazer in this unchartered territory, Dr. Carolina Tropini is helping unravel the mysterious world of bacterial communities in the intestines, leading her research team in a bid to seek a treatment, if not a cure, for IBD. A biophysicist and Assistant Professor in the School of Biomedical Engineering and the Department of Microbiology and Immunology at the University of British Columbia, Tropini won this year’s Johnson & Johnson Women in Science, Technology, Math, Manufacturing and Design Scholars Award in the field of engineering, a prize that includes a grant of US$150,000 and mentorship support for the next three years. Six winners were selected from 541 nominees worldwide. As a member of a small but growing number of pioneering women of science, Tropini is the first Canadian to be honoured with the award since its launch in 2017.
A delicately balanced ecosystem
IBD afflicts 270,000 Canadians – a number that’s expected to rise to 400,000 (about one percent of the population) by 2030 – and costs the healthcare system over $1.2 billion annually.
Dr. Tropini notes, “There’s this very interesting interplay between our lifestyle, the bacteria that we have in us, and our health.” Microbes in different parts of the bowel survive in delicately balanced ecosystems that can be disrupted severely by certain food and medicine, and other ailments like intestinal flu or colon cancer. These tiny critters live off nutrients passed through the bowel and in return, produce compounds that aid in digestion and guard against dangerous pathogens. Tropini believes there is even more to the story.
Her research team is studying the connection between the gut microbiota, the gut microenvironment and IBD. “Our goal is to further biological knowledge and to facilitate the development of methods that can predict disease state and drug effectiveness, as well as therapies for diseases that affect millions of people in the world,” Tropini explains.
Keeping gut microbes healthy protects against pathogens and prevents inflammation, but Tropini suggests current lifestyles are turning out to be detrimental to the microbiota. “Some of the things that have changed in our lifestyle is that not only do we have as much nutritional food for these bacteria, because we eat very processed foods, but we’re also losing them because we’re taking compounds like antibiotics and over-the-counter drugs that change the environment of the gut so strongly that we’re starting to lose a lot of these beneficial microbes,” she explains. “We’re really interested in understanding how changes in our gut environment affect the way that bacteria and viruses can survive.” She points out that viruses like COVID-19 are found in the digestive tract and that many patients show gastrointestinal symptoms even before they show the respiratory symptoms associated with the pandemic.
“I think that the impact of COVID-19 is going to be really important for a lot of different aspects of research. And one of the things that we know that’s related to the microbiota is that it’s very strongly affected by viruses attacking the gastrointestinal tract.”
Not without its challenges
“We are also trying to modify the microbial communities,” Tropini continues, “so that they will act in the way that we want. We’re looking from the perspective of dietary compounds. We think that by feeding the bacteria different compounds, we can help ameliorate this environment, so that it’s more able to support the growth and stability of bacteria that we think are beneficial.”
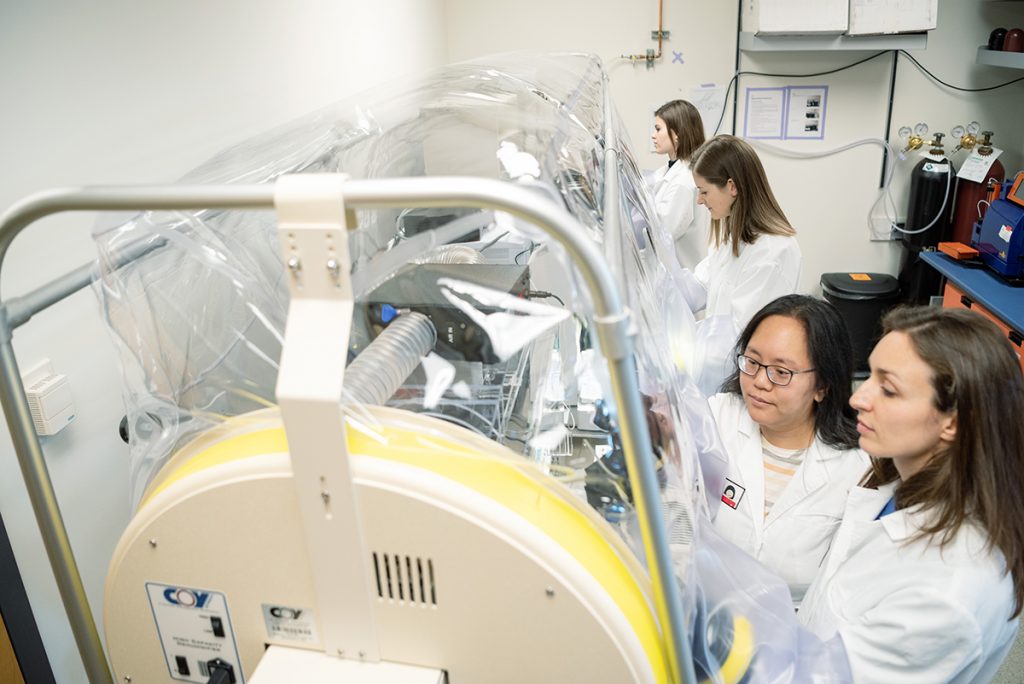
Working mostly with mouse intestines, the study of biopsies is not without its challenges, especially given the finicky nature of the mucus lining of the intestines, which harbours microbial communities. Live tissue from mouse intestines can be mounted in perfusion chambers or as colonic explants, but buffers and hydrating reagents must be applied very carefully to retain the natural thickness of the mucus. With electron microscopes, this was impossible because processing changed the mucus viscosity, and ultimately the ecosystem balance, that was seen through the device so it became scientifically irrelevant.
Grappling with these complexities, Dr. Tropini and her team rely on an arsenal of cutting-edge experimental and computational methods, using technologies often engineered internally with support from other university departments. “These are massive projects with a lot of different facets, so we work in very large, interdisciplinary teams,” she explains. “It requires interdisciplinary research, and I’ve been really lucky through my training to have been exposed to a lot of different types of techniques that come from very different fields like physics, all the way to microbiology, all the way to bioengineering.”
This includes using machine learning to integrate massive and diverse data sets to create predictive models and simulations. “For example, we will look at how a bacterium will respond to a change in the physical environment, or with the addition of a specific nutrient. And then we want to try to scale that understanding up to how it affects the health of the host.” Tropini explains that measuring the host’s immunological response is altogether different because it looks at how different cells change or whether the mucus layer is being affected.
Making science better
With the help of the three-year grant from the award, Dr. Tropini and her team hope to begin in vitro experiments that will shed light on which bacteria are creating environments that may lead to inflammation, and which may be preventing it. “Over the three years, we’re really trying to move into a position so we understand the system well enough that we can start to scale it up, and try to see whether we can move into something that will be more translational,” she says.
Down the road, Tropini’s team hopes to collaborate on novel therapies for IBD. She believes that science will get to a point in which understanding someone’s unique microbiota will lead to improved treatment and better health outcomes. “Where I see this going is personalized medicine – a lot of these diseases are incredibly different from person to person. By understanding this diversity, I hope that we’ll be able to target each person individually, and devise effective individual treatments.”
For now, Dr. Tropini is grateful for receiving the award, which she says opens up doors for women. She concludes, “There really needs to be more diversity, and there needs to be more inclusion, and there needs to be more voices to be heard, not only because it’s the right thing to do, but also because it makes science better.”
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community