UBC lab finds connection with Alzheimer’s disease
By Hermione Wilson
The Townsend Family Laboratories (TFL) at the University of British Columbia was established in July 2008 by founding director Weihong Song and with financial support from the David Townsend family. The main goal is to discover how genetic and non-genetic factors contribute to the development of Alzheimer’s disease and find new targets of Alzheimer’s drug development. The lab also focuses on the link between Alzheimer’s disease and Down’s syndrome.
“We’re basically looking for the molecular and cellular mechanism underlying how https://www.biolabmag.com/the-genetic-signpost/ people develop Alzheimer’s disease, and also how Alzheimer’s and dementia develop in [people with] Down’s syndrome,” says Song, Canada Research Chair in Alzheimer’s Disease and professor of psychiatry at UBC’s Faculty of Medicine. Almost all people with Down’s syndrome will develop typical Alzheimer’s neuropathology after middle age, Song says. That includes the development of neuritic plaque (also known as senile plaque), neurofibrillary tangles in the brain and Alzheimer’s-related dementia.
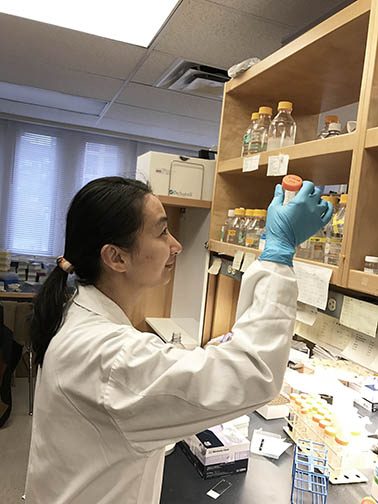
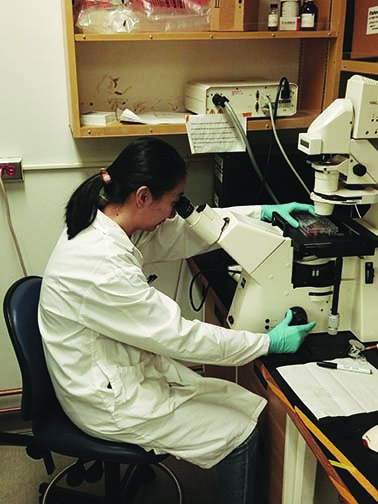
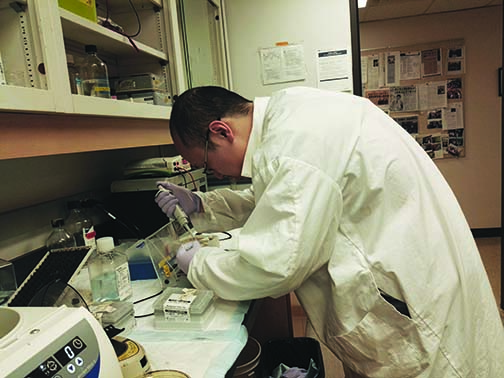
TFL is actually comprised of five labs including Genetic Lab for Neuropsychiatric Disorders, Lab for Animal Models of Neuropsychiatric Disorders, Molecular Biology Lab, Behavioural Lab, and Drug Development Lab.
As the lab is primarily involved in molecular and cellular work, it is equipped with PCR machines, genome sequencing machines and other tools necessary for the study of proteins and genes. There are also special behavioural testing facilities for the mice models of Alzheimer’s disease that the researchers work with. There are a total of 12 people working at the TFL, the majority of which are PhD students and post-doctoral fellows.
“What my lab has been doing for the past 25 years is really focus on how the beta amyloid – [which] is central to neuritic plaque formation – how that ABeta is being produced and how it is being cleared,” Song says. Beta Amyloid, or ABeta, is a peptide derived from a larger protein called the amyloid precursor protein (APP) and is a central component of neuritic plaque, he explains. The gene for encoding the amyloid precursor protein from which ABeta is derived also happens to be located on chromosome 21. Down’s syndrome is caused when a person is born with an extra copy of chromosome 21 and a rare form of Alzheimer’s known as early-onset familial Alzheimer’s disease (or FAD) – which occurs in less than 1 per cent of cases of Alzheimer’s disease – is caused by single-gene mutations on chromosomes 21, 14 and 1, specifically mutations in the Presenilin-1 and Presenilin-2 genes and the APP gene.
“What my lab has been doing is examining why those gene mutations cause Alzheimer’s disease development and looking for the impact on the ABeta production, because a mutation of the APP genes and the Presenilin genes could affect how APP is produced,” Song says.
Song and his fellow researchers at TFL hypothesize that understanding the mechanisms behind why ABeta accumulates in the brain and causes nerve death, leading to the development of Alzheimer’s, will allow them to control the production of the protein and perhaps prevent the formation of the neuritic plaque. The current hypothesis, Song says, is that the more APP that is produced, the more plaque that forms in the brain. The lab is currently looking at how genetic components affect APP production. The researchers have considered environmental factors such as low oxygen levels going to the brain, during a stroke for example, and traumatic brain injuries.
“Additionally we are looking for any potential treatments for Alzheimer’s disease,” Song says. “Previously, we published a study looking at the inhibitor of the enzyme that produces ABeta [as] a potential treatment.” The thinking is that if the activity of the enzyme could be inhibited and not allowed it to produce ABeta, the patient would not develop Alzheimer’s. In a recent study, published January 27, 2017 in Acta Neuropathologica, Song and his colleagues investigated the role of vitamin A deficiency in the development of Alzheimer’s disease.
Retinoic acid is an active component of vitamin A; it is also important for skin development, vision and the proper functioning of the immune system. “Vitamin A or retinoic acid has previously been shown to affect brain development,” Song adds.
The vitamin A study which he and his colleagues authored was based on a previous one where they surveyed 330 elderly people in Chongquing, China, and found that 75 per cent of those with mild or significant vitamin A deficiency had cognitive impairment, compared to 47 per cent of those with normal vitamin A levels.
In the more recent study, Song and his colleagues, in partnership with the Children’s Hospital of Chongquing Medical University (with whom the lab has been collaborating with for many years) looked at transgenic mouse models of Alzheimer’s. These mice have the Alzheimer’s phenotype or pathology, Song says; their brains already contain the neuritic plaque characteristic of the disease. When fed a diet low in vitamin A, pregnant mice gave birth to offspring who developed Alzheimer’s pathologies much earlier and whose cognitive function was lower than normal.
“That indicates that a vitamin A deficiency during pregnancy, in the womb, has a longlasting detrimental effect on the mice in terms of developing dementia at a later stage,” Song says. As to why low levels of vitamin A in the womb would cause cognitive deficits later in life, Song says it is thought that the corresponding low levels of retinoic acid, the active component in vitamin A, trigger more ABeta production, which leads to the forming of plaque in the brain.
While vitamin A deficiency is not as common in North America as it once was, it is still a prevalent health issue in some developing countries. According to the World Health Organization, an estimated 250 million preschool children are vitamin A-deficient.
In the vitamin A study, Song and his colleagues attempted to correct the effects of vitamin A deficiency in the newborn mice by feeding them a vitamin A supplement. Song says this led to some reversal of negative cognitive effects later on, but only when the vitamin A supplement was given early in the their lives at high doses.
Song is determined. “[My lab] is dedicated to finding the molecular and cellular mechanisms of Alzheimer’s and developing interventions to prevent and treat this devastating disease.”
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community