By Hermione Wilson
As with Ebola, Canadian researchers have once again stepped up to the plate, developing new and innovative ways to prevent, treat and vaccinate against the Zika virus. Although Zika may never reach Canadian shores, there has been a movement in the life science sector to rise to the challenge and provide help to countries that are struggling to contain it.
“We feel an obligation to mobilize in emerging infectious disease issues like Zika, because we can,” says Rick Galli, Chief Technical Officer at bioLytical. The British Columbia-based company is developing two new Zika detection methods, for which it has filed patents in the U.S. The Zika test is based on the company’s INSTI platform, which is geared to the detection of HIV.
BioLytical’s INSTI is an immunofiltration platform that is able to produce on-the-spot results in about 60 seconds. For the Zika virus, the company has developed two approaches: the first is a standard screening test that is sensitive to Zika but may also have some cross reactivity to other flaviviruses like Dengue, Galli says. That makes it ideal for populations who have never been exposed to the disease, he says, such as the U.S.
For areas in South America and the Caribbean where Zika and other flaviviruses have been prevalent for some time, a broad test doesn’t work as well, Galli says. That’s where the second approach comes in. “The second iteration [of the test] is to look for a specific IgM [Immunoglobulin M] marker which is present only in the acute phase of infection, so it’s more of a diagnostic tool as opposed to a screening tool,” he explains.
Dealing with the Ebola outbreak in 2013 and the ensuing scramble to develop an effective vaccine proved to be an instructive experience for regulatory bodies around the world. They have made sure that more funding opportunities and support are available this time around. In the U.S., the FDA has developed an emergency use regulatory process designed to prioritize Zika treatments, which Galli says bioLytical is aiming for. The World Health Organization has a similar process, called The WHO Emergency Use Assessment and Listing (EUAL) procedure.
The U.S. Health and Human Services’ Biomedical Advanced Research Development Authority (BARDA), as well as groups associated with the National Institutes of Health (NIH), have allocated priority funding to assist in the development of Zika treatments, Galli says.

In Canada, the Canadian Institutes for Health Research (CIHR), in partnership with the International Development Research Centre (IDRC), set up the Canada-Latin America-Caribbean Zika Virus Program in order to invest in groups developing diagnostics for the virus, researching the pathology of the virus, and working to prevent Zika’s transmission. Grand Challenges Canada, an organization that is fully funded by the government of Canada, teamed up with the Consortium for Affordable Medical Technologies (CAMTech) for a competition designed to accelerate the development and commercialization of innovations addressing the Zika crisis.
In May 2016, Grand Challenges Canada and CAMTech presented the Zika Innovation Awards, which recognized six innovative projects with a prize of $25,000 each. One of those recipients was Dr. Alex Brolo of the University of Victoria, for his low-cost biosensor for Zika screening. Brolo’s device uses nanoparticles of gold to detect the presence of the Zika virus in saliva.
“We basically prepare these gold nanoparticles, we immobilize them in glass, and then we coat the particles with a protein that is related to the Zika virus,” he says. “When you expose that strip… to the saliva of someone that is [infected], the antibodies that the person has in their saliva is going to attach to the surface. When this happens, there is a small colour change on the strip that we detect with a reader.”
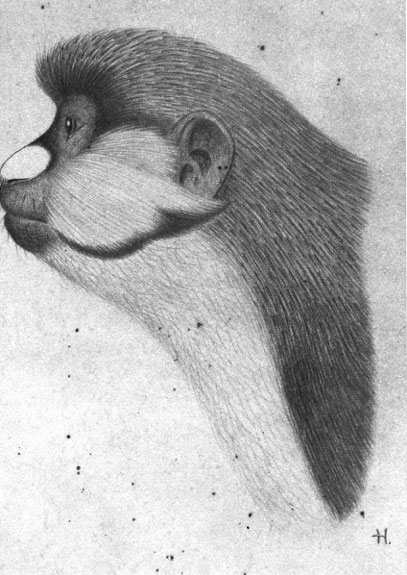
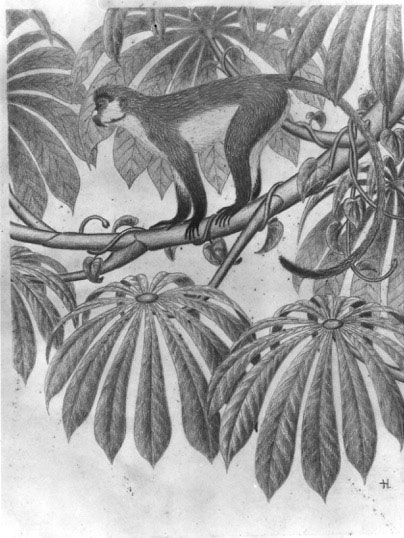
“Every year in Brazil is the same thing,” says Brolo, who grew up in Sao Paulo. “Summer starts, you start to see the news about the mosquitoes and it’s always the same thing going on over and over again.” He remembers health workers going from house to house looking for mosquitoes and handing out educational brochures.
“These diseases like Zika and Dengue and this kind of stuff, there is no specific treatment or vaccine or anything like that, so the solution for those things is to kill the mosquitoes,” he says. “That’s what people do and having been doing for the last 500 years.”
Brolo contemplated how he could make health workers’ jobs easier and improve the response time of the Brazilian government to these types of outbreaks. “These guys who go door to door… are not nurses or medical doctors or anything like that, so they cannot handle blood,” Brolo says. He knew he had to make his detection test easy to administer and give health workers the ability to get fast results. Using saliva instead of blood was one way of doing that; adding a geolocation feature to the device was another.
“The idea in the end is to do the reading of the result of the test on-site and hopefully get that connected to a cell phone, for example, that can upload the result in real-time… to generate a real-time map of the infection [and] how it is spreading,” he says.
The $25,000 grant from Grand Challenges Canada and CAMTech allowed Brolo and his team to develop a proof of concept, but their financial needs did not end there. They used that proof of concept to attract partners and investors who would help them reach the next stage of development, Brolo says. They hope to have Zika screening strips ready to send to Brazil for initial testing by the end of 2016.
Brolo and his group at the University of Victoria are also working with a group in the U.S. to develop a simple way to detect mosquito larvae, again incorporating a way to geolocate the position of mosquito breeding grounds. The detection method would involve taking a picture of standing water and using recognition software to identify what type of mosquito larvae were present. They received a separate Grand Challenges Canada grant for this project.
“The clinical protocol is a massive amount of information to assemble and submit to regulatory agencies,” Kobinger says. While Kobinger’s team was preparing the clinical protocol for both the FDA and Health Canada for the phase I human clinical trial, partners at the University of Pennsylvania were securing a strain of the virus through a pipeline they developed in Philadelphia, born out of their experience with West Nile Virus.
“On our side, we were advancing the animal model, knowing that at one point we would need to do what’s called a challenge experiment where we vaccinate the animal and then we expose them and infect them, and we can see if they’re protected or not,” Kobinger says of his team at Laval.
For Gary Kobinger, Director of the Infectious Disease Research Centre (IDRC) at Université Laval and leader of the first group to conduct human clinical trials on a Zika vaccine, the hardest part of developing a vaccine hasn’t been the clinical work, but the paperwork.
The Zika vaccine the Laval group is working on is being sponsored by Inovio Pharmaceuticals and GeneOne Life Science. Two other sites, at the University of Pennsylvania and the University of Miami, will also be conducting human clinical trials.
It was Kobinger and his colleague David Weiner of the University of Pennsylvania who first had the idea of developing a Zika vaccine. They started to seriously look into a vaccine in the fall of 2015, hoping to get something in the works before it became a problem in South America and the southern U.S.
“The vaccine is based on DNA that expresses only… a unit or part of the virus of interest,” Kobinger says. “[Weiner’s team] knew from West Nile studies which part of the virus was the most likely or promising in terms of making a vaccine.”
After three months of working separately on different aspects of the vaccine, the animal models were ready to go and they knew that the vaccine was immunogenic, meaning it generated an immune response, though they did not yet know whether it was protective or not. In the meantime, their clinical timeline was moving on schedule. Kobinger says they were able to accomplish all this, and get approval from the FDA and Health Canada, in about eight months. All in all, the process was smooth and rapid.
“What takes time is to assemble this package to submit our hundreds and hundreds of pages,” Kobinger says. “To assemble all the information related to a vaccine that is to be tested in humans is very demanding.”
He also notes that they weren’t able to get much financial support from agencies in Canada or the U.S. because of how early they started. In the U.S. there was an open call for Zika vaccines, Kobinger says, but the open call for vaccines in Canada came too late.
“I don’t mean this as a criticism,” he says. “Those funding opportunities take time for funding agencies to assemble.” Kobinger and his colleagues ended up organizing the three project sites in Quebec, Philadelphia and Miami with Inovio and GeneOne, without the help of any government agencies. Their commercial sponsors will bear the brunt of the vaccine development costs.
The response to calls for Zika treatments and vaccines has highlighted the work pharmaceutical and biotechnology companies are doing to support innovation in this area. This work isn’t always necessarily tied to a company’s bottom line, says Elizabeth Bailey, Director of CAMTech at the Massachusetts General Hospital Center for Global Health, but they do reap rewards in the form of reputation and greater relationships with stakeholders.
“They really recognize that they have an important role to play, partly in providing funding but also in providing engagement and expertise,” Bailey says of CAMTech’s commercial partners in the life science sector. “It’s been encouraging to see them take a more active role in things that don’t necessarily impact their business per se, but because they sit in the healthcare space, they want to be seen as being part of this broader coalition trying to make a difference and trying to address these different types of public health crises.”
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community