Medical genomics researchers aim to reduce impact of drug-induced hearing loss

By Robert Price
The situation is all-too-common and tragic. A middle-aged mother receives a diagnosis: She has ovarian cancer. The news knocks her over. It’s the hardest news that she and her family have ever faced. But they are determined. She will fight it, so she starts chemotherapy. Chemotherapy helps beat back cancer, but a side-effect of Cisplatin, one of the drugs, sideswipes her efforts: She’s lost some of her hearing. It started with a ringing in her ears, and now she has trouble hearing high-pitched frequencies. The cancer’s in remission. That’s good. But she feels diminished. She can’t hear everything she used to hear. And for somebody who loves music, the loss causes her great anguish.
This story isn’t unusual. Cisplatin has shown to be efficacious in fighting cancer but can cause hearing loss in up to 80 per cent of people who take the drug—a side effect that can devastate people already dealing with the devastations of cancer. Research indicates that genetics plays an important role in determining who is at risk of drug-induced hearing loss, with up to 50 per cent of hearing loss attributed to genetics. Young patients are particularly susceptible to hearing loss caused by the drug, and the effects can become a significant challenge for the many children who are treated with Cisplatin before they’ve developed language skills.
One person who hopes to solve the problem of drug-induced hearing loss is Dr. Britt Drögemöller, an assistant professor in the department of Biochemistry and Medical Genetics at the University of Manitoba and Canada Research Chair in Pharmacogenomics and Precision Medicine. Her lab works on identifying specific genetic variants that can help predict who’s going to experience hearing loss caused by Cisplatin and use that information to develop strategies to prevent it, such as using order protectants that, when taken in combination with Cisplatin, can help to prevent hearing loss without affecting the anti-cancer activity of the chemotherapy.
Two Approaches
Drögemöller uses two approaches in her studies to reduce the potential for hearing loss. In the first approach, her team collects genetic information for individuals who are receiving Cisplatin. They genotype the patients for around 400,000 genetic variants and then compare these variants to five million other variants spread throughout the genome. From this huge comparison, the lab identifies genetic variants that they think explain why some people experience the hearing loss. In the end, the lab produces a polygenic risk score, a measurement of a patient’s risk of hearing loss due to Cisplatin.
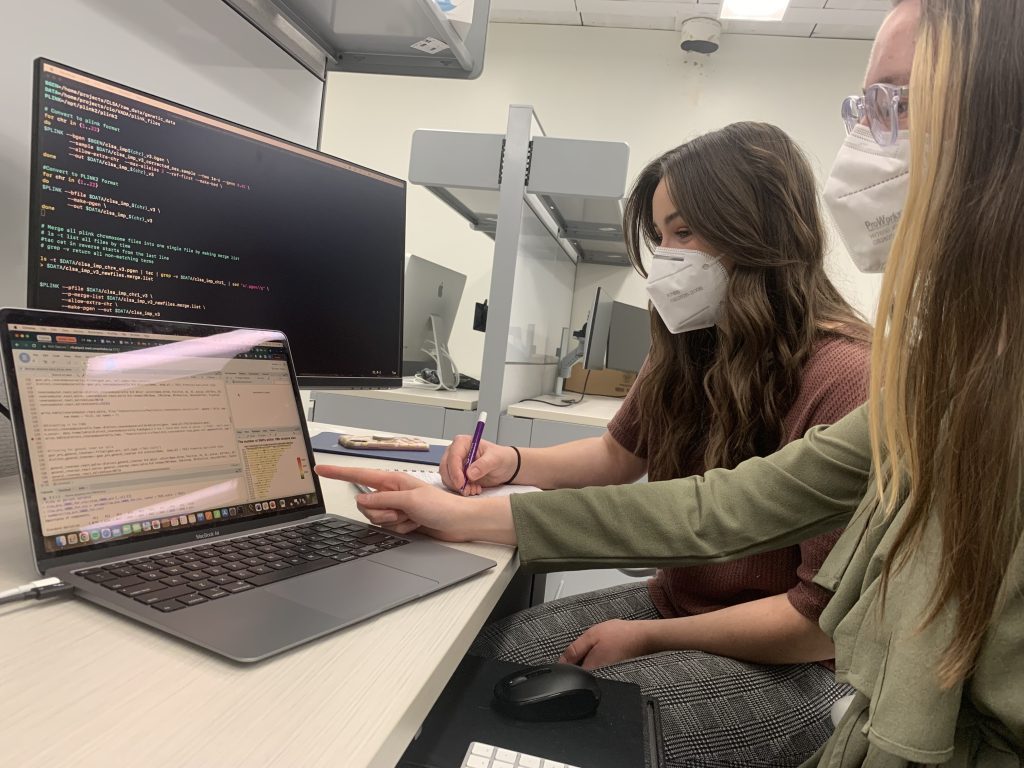
The analysis is all performed computationally, explains Drögemöller. “We can generate data really quickly these days and get a whole lot of data back all at once and get predictive information.”
The second approach uses a new technology called single cell sequencing to examine which cells might be at risk of death during chemo. Drögemöller came by this approach when she noticed Cisplatin causes gene expression changes in the ear. The problem is that it’s difficult to study changes in gene expression in the inner ear—the tissue in the inner ear is difficult to reach and the cells that make up that part of the ear’s structure are heterogeneous and complex. In fact, the most important cells in the inner ear—the hair cells that are dying because of Cisplatin treatment—only make up 1 to 3 per cent of all the cells in the ear. Until recently, researchers haven’t been able to look at these cells very easily. With Single Cell Sequencing, Drögemöller can generate gene expression information for each individual cell in the ear.
That’s exactly what her team is doing. Using mouse models of Cisplatin-induced hearing loss, she’s performing single cell sequencing on the mice to identify specific changes in gene expression that occur and hopefully understand what changes happen in the ear because of Cisplatin.
An Open Lab
Drögemöller describes her lab as “basically a computational lab.” A bank of computers conducts the analyses, and in the near future she hopes to bring in equipment that will allow her lab to perform the single cell sequencing experiments in-house.
The software driving Drögemöller’s analyses are all open source. That’s one of the great things about her field, she says, since it improves access to information. “The bioinformatics community is really big on making things easily accessible and shareable,” she says. This philosophy of open science—one where researchers around the world can all use the exact same programs, and share their code and analyses—means that somebody else can repeat the experiment without having to buy or license software. The goal of this openness is reproduction and confirmation of results. “We share all we use so that other people can repeat the analysis, and make sure that everything’s reproducible.”
This attitude has a revolutionary tinge to it, since many researchers still hold their discoveries close until they feel secure enough in their careers and businesses to disclose what they’ve found. Drögemöller says this attitude of secrecy is shifting, but slowly.
“I think there’s certainly a mentality that we need to share information and we need to make whatever we can share as easily accessible as possible. But for sure not everyone thinks like that,” she says. “I don’t think that’s really for the greater good. Especially in human genetics research, we need to have as much information as we can get. And the only way we can do that is by collaborating and sharing samples.”
Scaling back into larger knowledge
Drögemöller’s work scales back into a larger set of knowledge that has the potential to advance research across a range of situations. Hearing loss is a side effect of many drugs. Once she has her model set-up, she sees many easy ways to apply it to other drugs. “We even think that there’s common mechanisms behind drug-induced hearing loss,” she explains. “We’re interested to see if we see the same pathways involved in hearing loss when we look at other drugs. Or is it completely different if you have a different drug?”
Her team is also interested in understanding how age-related hearing loss comes about. More than 50 per cent of people over the age of 70 experience age-related hearing loss. Researchers are starting to see an overlap when they look at the genes and pathways that are involved in Cisplatin-induced, toxicity-related, or other forms of hearing loss. “If we can understand the biological mechanisms underlying hearing loss in general, we can really move forward to create strategies to prevent hearing loss from different drugs and from different environmental factors,” she explains.
In the long-term, Drögemöller’s work has the potential to add precision to medical interventions related to hearing loss. “In terms of precision medicine, the ultimate aim of this research is to generate genetic information for each individual and use that individual genetic information to predict how individuals will respond to different treatments before we apply them,” she says.
One day, researchers will be able to use a saliva sample or blood sample to collect genetic information from an individual before that person is prescribed Cisplatin, study the information to see how likely the patient is to experience hearing loss, and then use that information to develop new strategies and to create treatment plans suited to the individual.
“There are actually options these days where, for specific groups of patients, you can change the treatment plan slightly,” says Drögemöller, “and this is particularly helpful if you know that that patient’s at high risk of hearing loss.”
The sort of work Drögemöller is doing has other potential benefits, drug development in particular. Drug development is difficult. It’s like panning for gold: nuggets do appear, but most often that glint in the water is fool’s gold or a reflection of the sun. But the likelihood of success increases by about two-fold when genetic information, like knowing specific genes or pathways that contribute to specific diseases, is taken into account. Drögemöller’s approach generates knowledge about the biology underlying drug reactions and hearing loss, and this knowledge can help to guide how clinicians treat these side effects and even how researchers develop drugs.
The Future
The field of biochemistry and medical genetics have developed rapidly since Drögemöller started in the field, and these developments hold enormous potential for improving lives.
“When I started my research, I could only look at one genetic variant at a time,” she says. “Now we’ve got whole genome sequencing. We can look at sequencing in single cells. We can manipulate specific mutations.”
But the room to improve the precision of instrumentation is vast. Drögemöller says it’s still hard to work with sensitive samples, like cells in the inner ear. “We can do it, but we have to be very, very careful.” Technology that improves access to hidden parts of the body will energize research. When looking at things like gene expression, or epigenetic changes, technologies that are more robust and less influenced by the process to get the samples that will give researchers much more accurate data. “Which would be amazing,” she says.
“I think we’re getting there,” she adds. “The developments that have happened already, just while I’ve been in the field, are amazing.”
The speed of development, however, has slowed. Funding is scarcer than it was. Researchers are proposing safer projects most likely to receive backing. High-risk projects—those don’t get much attention. And that’s a problem, says Drögemöller, since it slows innovation across many disciplines.
But for now, Drögemöller says the recent innovations in her field have carved out an exciting space that researchers still haven’t fully exploited.
“Before we couldn’t even look at a lot of these things. And now we have the tools to do it, and I think it’s just a matter of mastering those tools and making sure they give us new insights into things.”
Lab Staff, Lab Funding
Drögemöller’s lab focuses predominantly on genetics, but the associates in the lab possess a range of skills that Drögemöller needs to perform the sensitive studies at the heart of her research. The geneticists in her lab collaborate with audiologists to understand the clinical side of how hearing loss actually occurs. Her interdisciplinary lab also employs experts in computation and biology. Drögemöller’s lab has received funding from CIHR, NSERC, local funding from Research Manitoba, the Health Sciences Foundation, and the Tri Council.
About Dr. Drögemöller
Britt Drögemöller, originally from South Africa, is Assistant Professor in the department of Biochemistry and Medical Genetics at the University of Manitoba and Canada Research Chair in Pharmacogenomics and Precision Medicine. She started her studies in the field of pharmacogenomics, a field that attempts to understand how genetic variants contribute to treatment outcomes. During her post-doc, she started working on the specific adverse drug reactions, an investigation that led her to look broadly at hearing traits. Today, her primary focus is human genomics, with a particular interest in using genetic information to understand why people respond differently to therapeutic treatments.
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community