Psychedelics company Numinus is betting on it
By Tracey Lindeman
Psychedelic drugs have been on one long, strange trip. From ritualistic and medicinal uses of peyote, ayahuasca and psilocybin mushrooms in Indigenous cultures throughout the Americas, to the CIA’s “mind control” experiments inside of MK-ULTRA, to the “turn on, tune in and drop out” era of recreational LSD, to now – the cutting edge of science in treating mental illness.
Not only treating mental illness, in fact, but maybe even curing it completely. That’s the next phase of the psychedelics journey, in which Canada is taking its first few, cautious steps.
“The end goal is psychedelic-assisted psychotherapy,” says Sharan Sidhu, science officer and general manager of Numinus Wellness, one of the Canadian private-sector players exploring the therapeutic elements of psychedelics.
With its home base in Vancouver and the newly acquired Mindspace Wellbeing psychology clinic in Montreal, the company is hoping to pioneer the use of mushrooms, ketamine, MDMA and other drugs to help solve the growing mental health crisis. If it can fully realize its vision, Numinus also will become a drug testing service provider to other companies in the expanding psychedelics arena, says Sidhu – “So really, setting the stage and setting the standard, while working with Health Canada to show them how it can be done… to be able to provide safe, effective therapy, but not at a huge cost.”
Psychedelics show promise
Health Canada is carefully recognizing the potential of psychedelics, especially when it comes to psilocybin. Last August, it gave four palliative care patients permission to use mushrooms. Four months later, it gave exemptions to 17 healthcare professionals affiliated with TheraPsil – a Canadian non-profit coalition advocating for psilocybin-assisted therapy – that allow them to use and possess mushrooms to understand its therapeutic possibilities. So far, TheraPsil says it has assisted 24 Canadians in accessing this kind of treatment.
One of the palliative care exemption holders, Thomas Hartle, has become a media fixture for his newfound advocacy of mushrooms. The Saskatoon man, who has Stage-4 colon cancer, took psilocybin under the guidance of Dr. Bruce Tobin at TheraPsil to help manage his illness-related anxiety. After just one session, Hartle described in a YouTube video feeling much less helpless and hopeless. “Having cancer feels like being dragged behind a horse,” he says in the video. “Maybe this would be a little closer to riding the horse.”
The mind is a complex yet delicate thing – a collection of cells, neurons, tissues and glands that control not only our physical reactions, but also our emotional ones. According to Canada’s Federal Framework on Posttraumatic Stress Disorder (PTSD), over three-quarters of Canadians “are exposed to one or more events within their lifetime that could cause psychological trauma.”
As the seminal book on PTSD, The Body Keeps the Score by Bessel Van der Kolk, argues, traumatic experiences leave imprints on our brains, and trauma can wreak havoc on our minds and bodies throughout our entire lives. There is a growing body of scientific evidence to support claims that psychedelic drugs help people overcome – or at least, alleviate symptoms of – PTSD, treatment-resistant depression, anxiety and substance use disorders, among other mental illnesses and disorders.
In a 2020 peer-reviewed article published in the International Journal of Neuropsychopharmacology, authors write that “PTSD remains a chronic illness, with high rates of psychiatric and medical comorbidity,” even when patients undergo psychotherapy. The authors studied four types of drugs: MDMA, ketamine, classical psychedelics such as psilocybin and LSD, as well as cannabinoids.
“Psychedelic drugs offer opportunities for a novel approach to the treatment of PTSD,” the authors conclude. “Each of the reviewed compounds provides a unique potential, from their use to rapidly target the symptoms of PTSD to their use as adjuncts to facilitate psychotherapeutic treatments.”

Addressing Canada’s mental health crisis
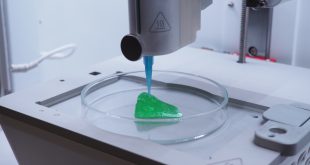
In a 7,000-sq.ft. lab on Vancouver Island, Numinus has a team of about a dozen scientists working on developing drug-testing methods, matrices and protocols, among other activities. In the company’s mycology room, where they grow mushrooms, only two people dressed in near-HAZMAT regalia are permitted at a time, to reduce potential for contamination.
The company is making big moves fast, with a number of acquisitions, partnerships and applications announced in recent months. In December, Numinus and the highly respected Multidisciplinary Association for Psychedelic Studies (MAPS) announced intentions to collaborate on a compassionate access trial in Canada to study MDMA’s effects on PTSD.
MAPS has heavy-hitting experience, running MDMA trials in the U.S. since 2019, after the drug was given a “breakthrough therapy designation” by the American Food and Drug Administration. MAPS expects to finish its report in 2022, with hopes of making a prescription treatment available the following year.
Advancements being made in the study of psychedelics come at a time when one in five Canadians experience mental illness or addiction. And, by the time Canadians turn 40, half of us will have, or have previously experienced, mental illness. Those two figures come from the Canadian Mental Health Association, which also says that 40 percent of Canadians have reported a decline in their mental health during the COVID-19 pandemic.
Dr. Devon Christie, a Vancouver-based family physician, joined Numinus as medical director in June for that very reason: to help industry push therapeutic psychedelics ahead faster than they would normally evolve within purely academic or scientific venues.
“Traditionally, it takes about 20 years for something that is proven to be efficacious in research to actually get translated into routine clinical practice, and we don’t have 20 years to wait for psychedelic-assisted psychotherapy to be adopted into clinical practice,” says Dr. Christie, pointing to the worsening rates of depression, anxiety and other mental and mood disorders.
“These are life-threatening conditions,” Dr. Christie continues. “People commit suicide and overdose. And not only can people die as a result of these conditions, but it’s also [about] the impact on people’s quality of life and their relationships with their families and communities, people who are out of the workforce – whereas these therapies actually show that in many cases, these conditions can actually be cured.”
For example, a small study by Johns Hopkins Medicine researchers tracked psilocybin use in 24 adults with major depression. “Four weeks post-treatment, 54 percent of participants were considered in remission – meaning they no longer qualified as being depressed,” the study, published in JAMA Psychiatry, notes.
The promise of a curative element feels both tempting and dangerous. As the Federal Framework on PTSD notes, many Canadians experiencing mental illness have long struggled to have their illnesses properly addressed, especially amid dire shortages of psychiatrists, high out-of-pocket therapy expenses and other barriers to mental health. Could taking a psychedelic drug once, twice, maybe three times at most – within a psychotherapy-assisted model, of course – really cure a person?
There’s only one way to find out.
SIDEBAR
Q&A with Health Canada
How many individual healthcare providers now have permission to use psychedelics in personal training?
Health Canada granted an exemption under subsection 56(1) of the Controlled Drugs and Substances Act (CDSA) to 19 healthcare professionals to use mushrooms containing psilocybin for the purpose of professional psilocybin-assisted psychotherapy training.
How many clinics have permission to use psychedelics?
No clinics have been granted an exemption from the CDSA to possess, provide or allow use of psilocybin. Exemptions for using mushrooms containing psilocybin for the treatment of end-of-life anxiety and psychological distress associated with a cancer diagnosis have been only granted to individual patients and to healthcare professionals for psilocybin-assisted psychotherapy training.
This being said, at this time psilocybin is authorized for use in one clinical trial and MDMA for use in seven clinical trials. Clinical trials authorized by Health Canada can be found here.
How many individual patients now have exempt status to use psychedelics for therapeutic reasons?
Health Canada granted an exemption under subsection 56(1) of the CDSA to 26 patients to use mushrooms containing psilocybin to treat their end-of-life anxiety and psychological distress associated with a cancer diagnosis. At this time, patients have only been granted subsection 56(1) of the CDSA exemptions to use mushrooms containing psilocybin.
What changes are being made to the special access program and other Health Canada programs to support research on psychedelics and psychedelic-assisted therapy?
Under the Food and Drugs Act, access to drugs that have not yet been approved for sale in Canada can typically be provided through either an approved clinical trial or through Health Canada’s Special Access Program (SAP).
As a result of regulatory changes made in 2013, access to restricted drugs (a category of substances that are controlled under the CDSA that have no approved medical uses) through the SAP is currently prohibited. MDMA, psilocybin and LSD are all restricted drugs. Ketamine, which does have approved medical uses, is not.
The SAP allows healthcare practitioners to better support patients with serious or life-threatening conditions by accessing drugs that have shown promise in clinical trials, or approved in other countries, but that have not yet been approved in Canada.
On December 12, 2020, Health Canada launched a 60-day public consultation seeking comments on a proposal to reverse the regulatory changes made in 2013 and thereby restore access to restricted drugs through the SAP. The department is currently reviewing the feedback received through this consultation, which closed on February 10, 2021. All feedback received will be carefully considered and will help determine whether or not to proceed with the proposed regulatory amendments.
Clinical trials remain the best mechanism to authorize the sale of restricted drugs (or any other unapproved drug) for the treatment of patients. However, there may be situations where patients are unable to participate in a clinical trial, for example when there are not any clinical trials available for a specific drug or in a specific area of the country. Restoring access to restricted drugs through the SAP would provide a potential option for healthcare professionals treating patients with serious or life-threatening conditions in instances where other therapies have failed, are unsuitable or are not available in Canada. However, restoring access through the SAP would not guarantee that applications to access restricted drugs would be approved. As is currently the case, all applications to the SAP would be considered on a case-by-case basis, taking into consideration the level of evidence pertaining to the safety, efficacy and quality of the drug, as well as the particular needs of the patient. For now, access to restricted drugs through the SAP remains prohibited.
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community