By Hermione Wilson
Ever since the federal Liberal government declared its intention to legalize marijuana (the dried leaves and flowers of the cannabis plant) discussion around the pros and cons of the controversial drug has been heating up.
On one hand, there are the therapeutic benefits of the cannabis plant when it is used to treat chronic pain, nausea, anxiety, spasticity, and a variety of other conditions. On the other hand, there are the plant’s psychoactive properties which make it popular for recreational use.
“I like to compare it to two rivers,” says Mark Ware, Director of Clinical Research at McGill University Health Centre’s Alan Edwards Pain Management Unit. “One is the patient knowledge that people have tried this for themselves and there’s a huge volume of patient-reported claims that cannabis helps with pain and sleep and spasticity and nausea and so on. The other river is the scientific understanding of the endocannabinoid system… that we have in our bodies, that appears to play an important role in the way that our bodies and our brains manage information, movement, memory, emotions, and so on. You put these two things together and it becomes a scientific rationale as to why it is that patients may report improvement in neuropathic pain. The challenge now is to bring those two rivers together and say, well, can we explore these claims with robust science.”
The compound that is responsible for marijuana’s psychoactive effect is delta-9-tetrahydrocannabinol (THC) and as researchers at the University of British Columbia have discovered, it has a very specific effect on decision-making.
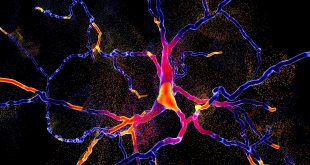
THC is a cannabinoid, a chemical compound derived from the cannabis plant that acts on and modifies the human brain’s endocannabinoid system. As with everything pertaining to the brain, the endocannabinoid system, a network of endogenous cannabinoid receptors, is very complex and little understood. As far as scientists can tell, at least one of those receptors, called CB1, acts as a necessary break in the process by which nerves connect and communicate with each other. When a nerve signal is passed from one nerve cell to the other, the nerve cell that is receiving the message sends a message back to the previous nerve saying that the message has been received and that there is no need to keep sending neurotransmitters. The cannabinoid system is integral in that process, Ware says.
“Once your nerve cells have communicated with each other, the cannabinoid system acts to suppress further activity, and that’s happening in everybody all the time,” he says. “We’re continuously using this system to keep our movements and our thoughts and our emotions smooth and controlled. When that system goes out of whack, then patients appear to need cannabinoids to help resume the normal endogenous tone of the cannabinoids.”
Catharine Winstanley is the senior author of a study out of UBC that investigated the effect THC had on rats’ ability to perform cognitively challenging tasks. The study found that while THC didn’t actually impair the rats’ ability to perform the tasks, it affected their willingness to complete the harder tasks. In other words, it made them lazy.
“It’s a very specific cognitive change, just a change in decision-making without the change in ability to do the demanding task,” Winstanley says. And THC seems to be the only cannabinoid that has this effect. Cannabidiol (CBD), the cannabinoid thought to be responsible for much of the therapeutic benefits of the plant, does not impair cognition at all.
“There are companies that are trying to create medicinal products based on cannabis that have higher levels of cannabidiol to THC in them and they’re suggesting that by increasing the level of cannabidiol they can overcome any negative effects of THC,” Winstanley says. “Unfortunately, when we tried to mimic that ratio, cannabidiol to THC, in our experiments – so giving equal amounts of both basically at the same time to the animals – we couldn’t stop THC from altering decision-making.”
“If we knew how THC works to alter cognition then maybe we could find a way of modulating it so that even if people did want to take the plant marijuana, then maybe we could provide them with a drug they could take at the same time that would stop THC from having bad effects,” she says.
Research like the UBC study is important, not just to patients who seek relief in medical marijuana, but to those who have developed a dependency on the drug. Winstanley and her colleagues are planning to join forces with researchers from the University of Toronto to explore the risk factors for addiction in young people and develop a cognitive assessment of people who are likely to abuse marijuana.
The cannabis plant has been used for centuries in a medicinal capacity, but because of its controversial nature and controlled substance status, research into why it has those beneficial effects have been stunted. It is very difficult to obtain cannabis for the purposes of research and requires special licenses that restrict the amount of cannabis researchers can possess.
“It normally takes around two to three years to get that license proposal deemed satisfactory by the government,” says Tegan Adams, Director of Business Development at Experchem Laboratories, a product testing facility in Ontario. “To get that approval you have to include as much detail as possible about what you’re doing at the site, and then when they come and visit, it needs to match up.” That slows down the research process considerably, as Larry Holbrook can attest to.
Holbrook is Chief Science Officer at Prairie Plant Systems (PPS), a plant biotech company and licensed producer of cannabis in Saskatchewan. The company has a pharmaceutical focus with a particular emphasis on purifying cannabis compounds and exploring different delivery methods such as oils. Prairie Plant Systems has been collaborating with CanniMed and researchers at McGill University and Dalhousie University on a clinical study looking at the ratio of THC to CBD that would be beneficial to pain relief in older patients with osteoarthritis. The trial was the first-ever to be approved and registered with Health Canada in 2014. Holbrook says Prairie Plant Systems is now in the process of recruiting patients.
Cannabis research in Canada may have been stunted by years of prohibition, but it is quickly gaining momentum. Holbrook knows of three clinical trials currently being set up in Canada: a study in Toronto looking into using cannabis to treat Tourette syndrome, another at the University of Guelph on cannabis’ anti-nausea effect, and a clinical trial in Saskatchewan looking at children with epilepsy. Ware mentions a Post-Traumatic Stress Disorder study that has been launched in British Columbia. “There certainly is a broad interest in trying to facilitate clinical research with cannabinoids in Canada,” Ware adds.
Part of the difficulty of doing clinical trials involving cannabis is the difficulty of obtaining materials for research and getting such a study approved by the government. The other barrier in researchers’ way, Holbrook says, is that there isn’t much financial support from the pharmaceutical industry.
“Pharmaceutical companies liked to have small drugs that they could synthesize and patent, in the past,” he says. “Something that is natural, from a plant, they never really liked because it didn’t give them a lot of intellectual property benefit.”
Still, the cannabis industry is clearly ripe for potential and with the prospect of a loosening, or at the very least a redefinition, of restrictions surrounding the substance, big pharma can’t help but take notice. If they have though, they’re playing it close to the chest, says Adams. “Until they actually have the results and publish them, or they’re useful, they’ll keep those data sets close to the chest,” she says. “They don’t want someone else to get it or figure out what they’re doing.”
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community