By Hermione Wilson
When a medical treatment is as effective as the stem cell therapy out of Ottawa has been, it’s not surprising that the press is throwing around the word “cure”. In 2001, researchers from The Ottawa Hospital and the University of Ottawa, led by Harold Atkins and Mark S. Freedman, treated 24 patients who had aggressive forms of multiple sclerosis with a stem cell transplantation technique originally developed to treat leukemia. They began by completely decimating the patients’ immune systems with chemotherapy and then transplanting them with their own newly purified hematopoietic stem cells in an effort to regenerate a new immune system.
The patients were followed for the next 13 years and what they observed was nothing short of remarkable. While a third of the patients continued to develop disabilities associated with rapid onset MS, the other two-thirds of patients either stabilized or saw improvements to their disabilities. Failing vision improved, mobility returned; one participant named Jennifer Molson went from using a wheelchair to skiing and getting her driver’s license. The treatment seemed to stop the inflammation caused by MS in its tracks.
Still, Atkins is hesitant to invoke the “c” word.
“A cure, for me, would be a patient living their life and never having a symptom or suffering from multiple sclerosis again,” he says. “We don’t know if this is a cure or not because our longest patient is only 13 or 14 years after her transplant, so time will tell. What we can say is the active inflammation has stopped and it has been controlled for a long time.”
A real cure, Atkins says, would mean no further damage caused by the immune system’s deranged attack on the brain. In fact, it would mean the damage would be repaired and everything would go back to normal. Of course, the results of the Ottawa trial are encouraging, but Timothy Caulfield is cautious in his praise.
“I’m always hesitant to use that word ‘cure,’” says the Canada Research Chair in Health Law and Policy and professor at the University of Alberta. “The results here have been very good but it’s a serious process. Here you have Harry [Atkins]’s approach where you completely ablated the immune system using chemotherapy… then the very specific and measured introduction of stem cells in a very particular kind of way, in a highly monitored clinical setting, versus a lot of these clinics where they’re just injecting stem cells – or who knows what they’re injecting – to treat the same condition.”
Caulfield is referring to the proliferation of unregulated stem cell clinics in countries where the regulatory framework is not as strict. These unscrupulous clinics offer supposedly miraculous stem cell treatments, based on unproven science, to mostly rich and desperate foreigners searching for a cure. It’s called stem cell tourism and the results can range from merely ineffective to potentially harmful. While the tantalizing promise of miraculous cures tempt patients overseas, it puts pressure on the industry here in North America to get effective therapies to the clinic faster, Caulfield says.
“I think that the science really isn’t there yet for most therapies and the work that’s been done by Harry [Atkins] and his team really shows the slow, and thankfully positive, progress of science towards the clinic.”
Despite it being early days yet, Canadian scientists have been steeped in stem cell research since their discovery at the Ontario Cancer Institute in Toronto in the 1960s. Continuing the work is a network of institutions and investigators intent on translating current stem cell research into working therapies and treatments. Besides the Ottawa MS trial, however, there haven’t been many that have made it to the clinic.
“The historic problem is we’ve got these discoveries to a point but then can’t take it beyond and actually commercialize the technology,” says Michael Israels, CFO of Centre for Commercialization of Regenerative Medicine (CCRM), of Canadian stem cell research. “We have funding in the early stages… but as you go along, industry at the back end, pharma and other large organizations, are happy to spend money on things that are close to being able to go to market.”
Israels is hoping a recent allocation of funds from the federal government will change that. The government announced in January that it would be committing $20 million to CCRM to help build a stem cell therapy development facility in Toronto, and GE Healthcare is matching those funds with another $20 million. Alongside the new facility, Israels says, CCRM plans to build a cell manufacturing facility that will focus on manufacturing human cells for clinical trial use.
In March, the Canadian government’s 2016 budget allocated $12 million over two years to support the Stem Cell Network’s research, training and outreach activities, according to a press release from the Canadian Stem Cell Foundation. The release goes on to say that a coalition of Canadian stem cell scientists, clinicians, business leaders, health charities and philanthropists have outlined a plan to deliver “up to 10 new curative therapies within 10 years,” according to a proposed Canadian Stem Cell Strategy.
Bold words, but can the Canadian stem cell sector back them up? The stem cell transplantation technique used by Atkins and his colleagues in Ottawa has certainly borne fruit, albeit after several decades of development.
“The technology that we’re using for hematopoietic stem cell transplantation took 20 years to become mainstream, from the time it was thought of to treat leukemia, to when it really started to be used broadly,” Atkins says. “I think these other stem cell [therapies will] have the same learning curve. I think it will happen but I don’t think it will happen overnight.”
Photo credits
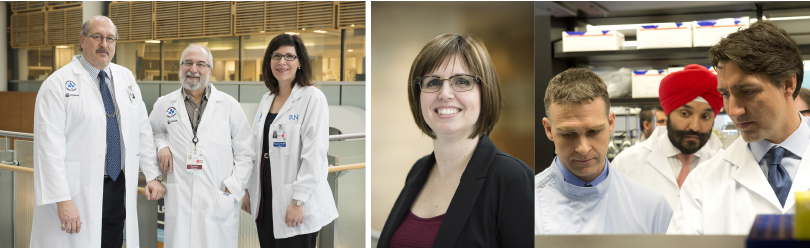
Photo credit: Prime Minister Justin Trudeau pledges his government’s financial support for a centre of advanced therapeutic cell technologies in Toronto. Photo credit: Canadian Press Images/CCRM/Salvatore Sacco
Left: Ottawa Hospital Research Institute researchers Mark S. Freedman, Harold Atkins and Marjorie Bowman were part of a $6.47-million trial that used blood stem cells to regenerate the immune systems of people with early, aggressive multiple sclerosis (MS).
Center: Jennifer Molson, an MS sufferer who saw dramatic improvements in her condition, was one of that trial’s most successful participants.
Highlights from U of T
The University of Toronto is pulling its weight in the stem cell space, with a number of projects underway. CCRM is collaborating with ExcellThera Inc. on a technique that uses technology from U of T to expand the volume of hematopoietic stem cells in umbilical cord blood so that it can be used in adult leukemia patients. Clinical trials are currently in progress.
Meanwhile, U of T biomedical engineer Molly Shoichet and her colleagues Derek van der Kooy and Valerie Wallace have been investigating the use of stem cells in treating blindness. Shoichet’s work involves bioengineering cell delivery platforms that will ensure the survival of these cells when they are injected into the patient. Their research has shown some functional improvement in mouse models of blindness after the injection of rod photoreceptor cells derived from adult retinal stem cells.
“What we’re trying to do is come up with a strategy that will actually reverse blindness,” Shoichet says.
Shoichet is also collaborating on stroke research with Professors Cindi Morshead, Andras Nagy and Dale Corbett. They have observed some functional repair after delivering neuronal cells derived from human induced pluripotent stem cells to the brains of rat models of stroke.
 BioLab Business Magazine Together, we reach farther into the Canadian Science community
BioLab Business Magazine Together, we reach farther into the Canadian Science community